Abstract
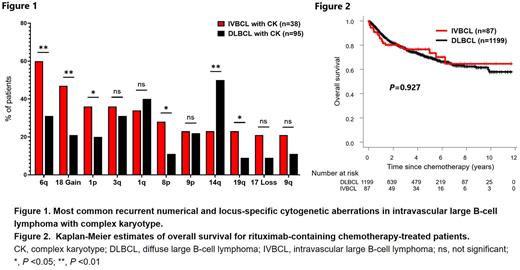
[Introduction] Intravascular large B-cell lymphoma (IVBCL) is a rare subtype of diffuse large B-cell lymphoma (DLBCL), aggressive behavior, and is often diagnosed postmortem. Although application of rituximab-containing chemotherapy (R-chemo) improved prognosis, diagnosis of IVBCL is still challenging. Due to insufficient sensitivity of biopsy and unspecific symptoms, some IVBCL cases require repeated biopsies without confidence in the diagnosis. Thus, identifying clinical findings specific to IVBCL is beneficial for real-world practice. Since some IVBCL cases showed complex karyotype (CK) in the bone marrow (BM) without histologically proven involvement, we hypothesized that this finding might provide a clue to the diagnosis of IVBCL. [Methods] We retrospectively evaluated patients with histopathologically proven newly diagnosed IVBCL or DLBCL according to the World Health Organization criteria between January 2010 through February 2022 from hospitals participating in the North Japan Hematology Study Group (NJHSG). BM biopsies were conducted at the time of the initial diagnosis. According to the BM results, the cases were dichotomized into those with histological BM involvement (BMIhisto+) and those without (BMIhisto-). Conventional cytogenetic tests using the G-banding technique were performed on BM aspirates. The karyotypes were recorded according to the International System for Human Cytogenetic Nomenclature. CK was defined as ≥3 chromosomal abnormalities. Event free survival (EFS) was defined as the time from the start of treatment to the first of: progression, relapse, initiation of a new line of treatment, or death from any cause. [Results] A total of 1945 DLBCL (age 19-109 years, median 71 years) and 106 IVBCL cases (age 30-92 years, median 69 years) were identified. BM biopsy and cytogenetic test were performed in 1481 and 1432 DLBCL cases and 100 and 96 IVBCL cases, respectively. 179 DLBCL and 41 IVBCL cases were BMIhisto+ (12.1% vs. 41.0%, P < 0.0001). Chromosomal abnormalities and CK were detected in 182 and 95 DLBCL cases while found in 47 and 38 IVBCL cases, respectively (chromosomal abnormality; 12.3% vs. 49.0%, P < 0.0001, CK; 6.7% vs. 39.6%, P < 0.0001). In patients classified with BMIhisto- who performed both BM biopsy and chromosome analysis, 21 of 1069 in DLBCL and 12 of 58 in IVBCL showed CK (2.0% vs. 20.7%, P < 0.0001). Most common recurrent numerical and locus-specific cytogenetic aberrations in IVBCL cases with CK are presented in Fig.1. Compared with DLBCL, IVBCL exhibited different pattern in some numerical and structural chromosomal aberrations. Next, we evaluated the survival of the 1199 DLBCL and 87 IVBCL cases who received R-chemo, and underwent both BM biopsy and chromosome analysis. The two groups did not have significant differences in age or sex distribution. Decreased general conditions (ECOG PS ≥2) and elevated LDH levels were found at significantly higher rates in IVBCL cases than in DLBCL cases. Median follow-up duration for censored cases was 47.6 months (range, 0.4-140.4 months) in DLBCL cases and 44.1 months (range, 1-140.5 months) in IVBCL. Overall survival (OS) and EFS in DLBCL cases were equal to those in IVBCL (5-year OS; 69.5% vs. 73.4%, P = 0.927, Fig.2, 5-year EFS; 54.1% vs. 61.4%, P = 0.243). In DLBCL cases, presence of CK significantly correlated with worse OS and EFS in both BMIhisto+ (median OS; 16.8 months vs. 117.4 months, P < 0.001, median EFS; 7.2 months vs. 27.9 months, P < 0.001) and BMIhisto- groups (median OS; 33.5 months vs. not reached, P < 0.0001, median EFS; 8.8 months vs. 93.8 months, P < 0.0001). However, in IVBCL cases, CK did not correlated with poor prognosis in both BMIhisto+ (median OS; not reached vs. not reached, P = 0.691, median EFS; not reached vs. not reached, P = 0.309) and BMIhisto- groups (median OS; 74.9 months vs. not reached, P = 0.853, median EFS; 30.6 months vs. not reached, P = 0.359). [Conclusion] In this study, we showed that incidentally detected CK in the BM was observed in about 20% of BMIhisto- IVBCL. Interestingly, IVBCL showed a distinct pattern of chromosomal abnormalities from DLBCL. Moreover, we showed that the prognosis of R-chemo-treated IVBCL was not inferior to that of DLBCL. Although the presence of CK itself does not directly affect the prognosis of IVBCL, for the cases that require repeated biopsies, this finding may increase the sensitivity of the BM test leading to further improvement of the potential prognosis.
Disclosures
Horiguchi:Janssen Pharmaceutical KK: Honoraria; AstraZeneca KK: Honoraria; AbbVie GK: Honoraria. Teshima:Fuji Pharma: Research Funding; Luca Science Inc.: Research Funding; Bristol-Myers Squibb: Honoraria; Novartis: Membership on an entity's Board of Directors or advisory committees, Other: Manuscript preparation, Research Funding; NIPPON SHINYAKU: Research Funding; Janssen: Other: Manuscript preparation; Astellas: Research Funding; TEIJIN PHARMA: Research Funding; Chugai: Research Funding; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria; Merck Sharp & Dohme: Honoraria, Membership on an entity's Board of Directors or advisory committees; Sanofi: Research Funding; Kyowa Kirin: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal